Malaria transmission structure in the Peruvian Amazon through antibody signatures to Plasmodium vivax
Jason RosadoID1,2,3*, Gabriel Carrasco-EscobarID4,5, Oscar NolascoID6,7, Katherine GarroID7 , Hugo Rodriguez-Ferruci8 , Mitchel Guzman-GuzmanID9 , Alejandro Llanos-CuentasID6 , Joseph M. VinetzID6,9,10, Narimane Nekkab1 , Michael T. White1,3, Ivo Mueller1,11,12☯, Dionicia GamboaID6,9,13☯
1 Unit of Malaria: Parasites and hosts, Institut Pasteur, Paris, France, 2 Sorbonne Universite´, ED 393, Paris, France, 3 Infectious Disease Epidemiology and Analytics G5 Unit, Institut Pasteur, Paris, France, 4 School of Public Health, University of California San Diego, La Jolla, California, United States of America, 5 Health Innovation Laboratory, Instituto de Medicina Tropical Alexander von Humboldt, Universidad Peruana Cayetano Heredia, Peru, 6 Instituto de Medicina Tropical Alexander von Humboldt, Universidad Peruana Cayetano Heredia, Lima, Peru, 7 Laboratorio de Malaria, Laboratorios de Investigacio´n y Desarrollo, Facultad de Ciencias y Filosofı´a, Universidad Peruana Cayetano Heredia, Lima, Peru, 8 Universidad Nacional de la Amazonı´a Peruana, Loreto, Peru, 9 Laboratorio ICEMR-Amazonia, Laboratorios de Investigacio´n y Desarrollo, Facultad de Ciencias y Filosofı´a, Universidad Peruana Cayetano Heredia, Lima, Peru, 10 Section of Infectious Diseases, Department of Internal Medicine, Yale School of Medicine, New Haven, Connecticut, United States of America, 11 Department of Medical Biology, University of Melbourne, Melbourne, Australia, 12 Population Health and Immunity Division, Walter and Eliza Hall Institute of Medical Research, Melbourne, Australia, 13 Departamento de Ciencias Celulares y Moleculares, Facultad de Ciencias y Filosofı´a, Universidad Peruana Cayetano Heredia, Lima, Peru
☯ These authors contributed equally to this work.
* javier.rosado@pasteur.fr
Abstract
Background
The landscape of malaria transmission in the Peruvian Amazon is temporally and spatially heterogeneous, presenting different micro-geographies with particular epidemiologies. Most cases are asymptomatic and escape routine malaria surveillance based on light microscopy (LM). Following the implementation of control programs in this region, new approaches to stratify transmission and direct efforts at an individual and community level are needed. Antibody responses to serological exposure markers (SEM) to Plasmodium vivax have proven diagnostic performance to identify people exposed in the previous 9 months.
Methodology
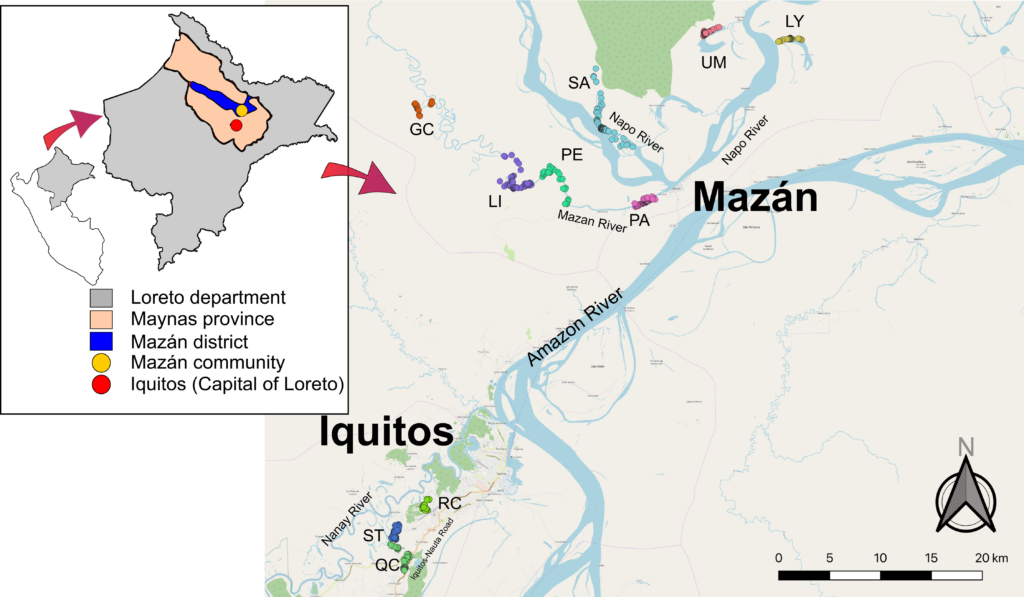
We measured antibody responses against 8 SEM to identify recently exposed people and determine the transmission dynamics of P. vivax in peri-urban (Iquitos) and riverine (Mazán) communities of Loreto, communities that have seen significant recent reductions in malaria transmission. Socio-demographic, geo-reference, LM and qPCR diagnosis data were collected from two cross-sectional surveys. Spatial and multilevel analyses were implemented to describe the distribution of seropositive cases and the risk factors associated with exposure to P. vivax.
Principal findings
Low local transmission was detected by qPCR in both Iquitos (5.3%) and Mazán (2.7%); however, seroprevalence indicated a higher level of (past) exposure to P. vivax in Mazán (56.5%) than Iquitos (38.2%). Age and being male were factors associated with high odds of being seropositive in both sites. Higher antibody levels were found in individuals >15 years old. The persistence of long-lived antibodies in these individuals could overestimate the detection of recent exposure. Antibody levels in younger populations (<15 years old) could be a better indicator of recent exposure to P. vivax.
Conclusions
The large number of current and past infections detected by SEMs allows for detailed local epidemiological analyses, in contrast to data from qPCR prevalence surveys which did not produce statistically significant associations. Serological surveillance will be increasingly important in the Peruvian Amazon as malaria transmission is reduced by continued control and elimination efforts.
Author summary
A challenge for eliminating Plasmodium vivax is its relapsing nature that can contribute up to 80% of the P. vivax cases. The detection of this source of transmission remains crucial for focused interventions in settings attempting to achieve elimination. Antibody responses to serological exposure markers to P. vivax have been validated to detect recent exposure and likely hypnozoite carriers in low transmission settings. To evaluate the benefits of adding serology to the detection of infection in areas where malaria transmission is rapidly reduced, we measured the prevalence of P. vivax by qPCR and serology in two sites of the Peruvian Amazon. This study shows that antibody responses to P. vivax antigens can detect more recently exposed people than molecular testing, providing more statistical power for surveillance and critical additional epidemiological knowledge for regions attempting to eliminate malaria transmission.