Malaria Molecular Surveillance in the Peruvian Amazon with a Novel Highly Multiplexed Plasmodium falciparum AmpliSeq Assay
Nueva Publicación de nuestros investigadores Carlos Fernandez Miñope, Christopher Delgado Ratto y Dionicia Gamboa Felicitamos a los investigadores de Instituciones Colaboradoras Institute of Tropical Medicine Antwerp Johanna Helena Kattenberg, Nobert Van Dijk, Pieters Guetens, Eduard Rovira Vallbona, Pieter Monsieurs y Anna Rosanas Urgell University of Antwerp Jean-Pierre Van Geertruyden U.S. Naval Medical Research Unit No. 6 (NAMRU-6): Hugo Valdivia Año:2023 […]
Nueva Publicación de nuestros investigadores
Carlos Fernandez Miñope, Christopher Delgado Ratto y Dionicia Gamboa
Felicitamos a los investigadores de Instituciones Colaboradoras
Institute of Tropical Medicine Antwerp Johanna Helena Kattenberg, Nobert Van Dijk, Pieters Guetens, Eduard Rovira Vallbona, Pieter Monsieurs y Anna Rosanas Urgell
University of Antwerp Jean-Pierre Van Geertruyden U.S. Naval Medical Research Unit No. 6 (NAMRU-6): Hugo Valdivia
Año:2023 Revista:Microbiology Spectrum SJR:2.15 Q:1
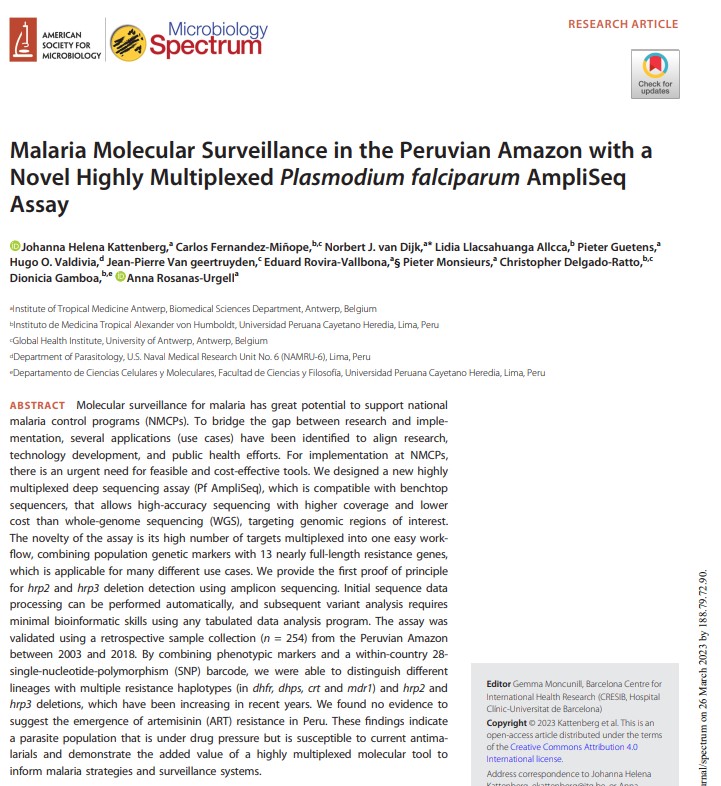
Malaria Molecular Surveillance in the Peruvian Amazon with a Novel Highly Multiplexed Plasmodium falciparum AmpliSeq Assay
Johanna Helena Kattenberg 1, Carlos Fernandez-Miñope 2 3, Norbert J van Dijk 1, Lidia Llacsahuanga Allcca 2, Pieter Guetens 1, Hugo O Valdivia 4, Jean-Pierre Van Geertruyden 3, Eduard Rovira-Vallbona 1, Pieter Monsieurs 1, Christopher Delgado-Ratto 2 3, Dionicia Gamboa 2 5, Anna Rosanas-Urgell 1
Affiliations
- Institute of Tropical Medicine Antwerp, Biomedical Sciences Department, Antwerp, Belgium.
- Instituto de Medicina Tropical Alexander von Humboldt, Universidad Peruana Cayetano Heredia, Lima, Peru.
- Global Health Institute, University of Antwerp, Antwerp, Belgium.
- Department of Parasitology, U.S. Naval Medical Research Unit No. 6 (NAMRU-6), Lima, Peru.
- Departamento de Ciencias Celulares y Moleculares, Facultad de Ciencias y Filosofía, Universidad Peruana Cayetano Heredia, Lima, Peru.
- PMID: 36840586
- DOI: 10.1128/spectrum.00960-22
Abstract
Molecular surveillance for malaria has great potential to support national malaria control programs (NMCPs). To bridge the gap between research and implementation, several applications (use cases) have been identified to align research, technology development, and public health efforts. For implementation at NMCPs, there is an urgent need for feasible and cost-effective tools. We designed a new highly multiplexed deep sequencing assay (Pf AmpliSeq), which is compatible with benchtop sequencers, that allows high-accuracy sequencing with higher coverage and lower cost than whole-genome sequencing (WGS), targeting genomic regions of interest. The novelty of the assay is its high number of targets multiplexed into one easy workflow, combining population genetic markers with 13 nearly full-length resistance genes, which is applicable for many different use cases. We provide the first proof of principle for hrp2 and hrp3 deletion detection using amplicon sequencing. Initial sequence data processing can be performed automatically, and subsequent variant analysis requires minimal bioinformatic skills using any tabulated data analysis program. The assay was validated using a retrospective sample collection (n = 254) from the Peruvian Amazon between 2003 and 2018. By combining phenotypic markers and a within-country 28-single-nucleotide-polymorphism (SNP) barcode, we were able to distinguish different lineages with multiple resistance haplotypes (in dhfr, dhps, crt and mdr1) and hrp2 and hrp3 deletions, which have been increasing in recent years. We found no evidence to suggest the emergence of artemisinin (ART) resistance in Peru. These findings indicate a parasite population that is under drug pressure but is susceptible to current antimalarials and demonstrate the added value of a highly multiplexed molecular tool to inform malaria strategies and surveillance systems. IMPORTANCE While the power of next-generation sequencing technologies to inform and guide malaria control programs has become broadly recognized, the integration of genomic data for operational incorporation into malaria surveillance remains a challenge in most countries where malaria is endemic. The main obstacles include limited infrastructure, limited access to high-throughput sequencing facilities, and the need for local capacity to run an in-country analysis of genomes at a large-enough scale to be informative for surveillance. In addition, there is a lack of standardized laboratory protocols and automated analysis pipelines to generate reproducible and timely results useful for relevant stakeholders. With our standardized laboratory and bioinformatic workflow, malaria genetic surveillance data can be readily generated by surveillance researchers and malaria control programs in countries of endemicity, increasing ownership and ensuring timely results for informed decision- and policy-making.
Keywords: DNA sequencing; Plasmodium falciparum; drug resistance; genetic epidemiology; hrp2 and hrp3 deletions; malaria; surveillance studies.

FIG 1 Annual P. falciparum cases in Peru (black line) from 1992 to 2020, with first-line treatment policy changes (data from the Centro Nacional de Epidemiología, Prevención y Control de Enfermedades [2020] Sistema de Atención de Solicitudes de Acceso a la Información Pública vía Internet del Ministerio de Salud [available at http://www.minsa.gob.pe/portada/transparencia/solicitud/]). Artemisinin combination therapies (ACTs) were first introduced into the Amazon region in Peru in 1999 and the North Coast in 2001, contributing to a dramatic decline in the number of cases. The combination of artesunate, mefloquine, and primaquine (AS+MQ+PQ) was the recommended first-line treatment in the Amazon region from the start (51), with continued high efficacy (107), and the combination of AS plus sulfadoxine-pyrimethamine (SP) was used on the North Coast. In 2015, AS+MQ+PQ became the recommended first-line treatment in the whole country (108). Peru reduced the malaria case incidence by ≥40% by 2010 using passive case detection (PCD), diagnosis by light microscopy (LM), and treatment with AS+MQ as the main components of the control program (109). In 2015, with the realization that PCD missed asymptomatic infections (110), focal screening and treatment were introduced, resulting in a further reduction in the malaria incidence (50). CQ+PQ, chloroquine plus primaquine; QN, quinine.

FIG 4 Dynamics of 28-SNP-barcode multilocus lineages. An area plot shows the proportions of each ML lineage detected in the three different time periods in study samples (n = 254) from Peru. ML lineages were identified, clustered using the genetic distance between barcodes with the poppr package in R, and given an identification number. ML lineages differed by multiple SNPs (≥4 SNPs), enabling lineage classification even when barcodes had some missing or heterozygous genotypes. Lineages are characterized by unique barcodes and resistance genotypes and are listed in Table 2.